Introduction
Gingivitis vs Periodontitis health is crucial to overall well-being, yet it is often overlooked. Conditions like gingivitis and periodontitis are among the most common dental issues worldwide, but many people fail to understand their significance or the differences between them. Gingivitis vs Periodontitis represents the earliest stage of Gingivitis vs Periodontitis disease, while periodontitis is a more advanced and severe condition that can lead to tooth loss and other complications. By identifying these conditions early and understanding their distinctions, you can take actionable steps to preserve oral health. This comprehensive guide sheds light on these two gum diseases, their causes, treatments, and preventive measures.
What is Gingivitis?
Definition and Characteristics
Gingivitis vs Periodontitis is a mild, early-stage gum disease characterized by inflammation of the gums. The condition is often painless, so it frequently goes unnoticed until it worsens. Symptoms include red, swollen gums that bleed easily during brushing or flossing. While gingivitis does not cause permanent damage to the gums or teeth, untreated cases can progress to periodontitis, leading to severe oral health issues.
Causes and Risk Factors
The primary cause of Gingivitis vs Periodontitis is plaque, a sticky film of bacteria that forms on the teeth. If not removed through proper oral hygiene, plaque hardens into tartar, irritating the gums. Risk factors for gingivitis include poor brushing habits, smoking, hormonal changes, and certain medications that reduce saliva production. Addressing these factors can significantly reduce the likelihood of developing gingivitis.
Diagnosis
Dentists typically diagnose Gingivitis vs Periodontitis during routine check-ups. They assess gum health by checking for redness, swelling, and bleeding. Early detection is critical, as gingivitis is reversible with timely intervention. Ignoring symptoms can result in the disease progressing to periodontitis.
Treatment Options
Treating Gingivitis vs Periodontitis involves professional dental cleaning to remove plaque and tartar. Equally important is maintaining a consistent oral hygiene routine, including brushing twice daily, flossing, and using an antimicrobial mouthwash. These practices ensure that your gums remain healthy and free from further irritation.
What is Periodontitis?
Definition and Characteristics
Periodontitis is a severe form of gum disease that occurs when gingivitis is left untreated. This condition damages the soft tissue and bone that support the teeth, leading to gum recession, tooth mobility, and eventually tooth loss. Persistent bad breath and abscesses are other common signs of periodontitis.
Causes and Risk Factors
Periodontitis often develops as a result of untreated gingivitis. Factors such as smoking, poor oral hygiene, genetic predisposition, and systemic diseases like diabetes increase the risk. Chronic inflammation from periodontitis can also have systemic effects, linking it to heart disease and other health issues.
Diagnosis
Diagnosing periodontitis requires a thorough examination by a dentist or periodontist. They measure the depth of gum pockets and may take X-rays to determine bone loss. Advanced diagnostics help in tailoring an effective treatment plan.
Treatment Options
Treatment for periodontitis ranges from non-surgical methods, such as scaling and root planing, to surgical interventions like flap surgery or bone grafting. Antibiotics may also be prescribed to control infection. Post-treatment maintenance, including regular dental visits and meticulous oral hygiene, prevents recurrence.
Key Differences Between Gingivitis and Periodontitis
Symptoms
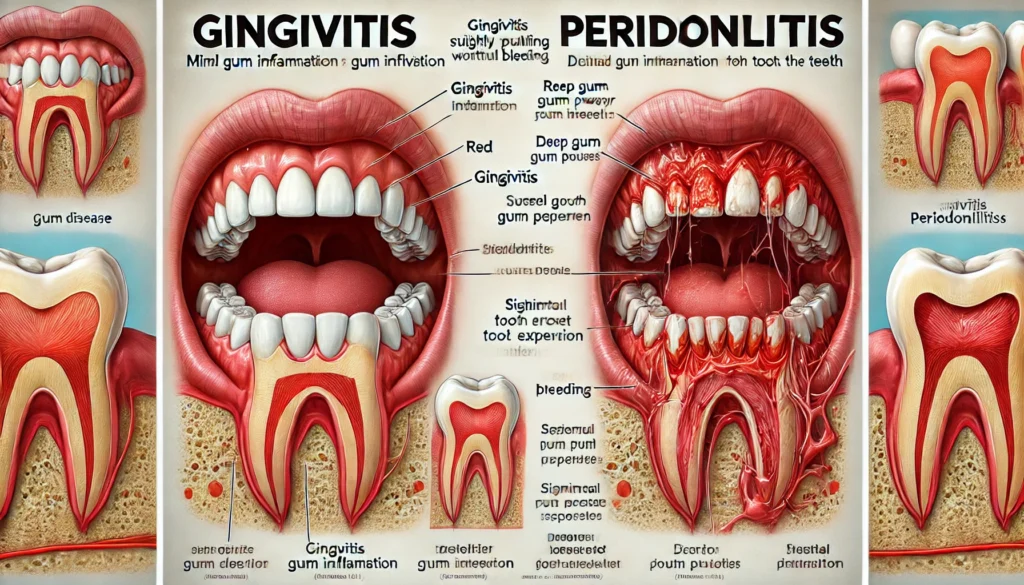
While gingivitis is marked by mild inflammation, periodontitis exhibits severe symptoms, including gum recession, tooth mobility, and persistent bad breath. A visual comparison reveals that periodontitis involves irreversible damage, whereas gingivitis can be adequately reversed.
Disease Progression
Gingivitis is a precursor to periodontitis. When untreated, the bacterial infection spreads beneath the gum line, damaging supporting structures. Periodontitis progresses in stages, from mild to advanced, each causing more destruction.
Treatment Intensity
Gingivitis treatment is straightforward and noninvasive, focusing on plaque removal and improved oral hygiene. In contrast, periodontitis requires more intensive and often invasive treatments, including surgery and long-term maintenance.
Impact on Overall Health
Both gingivitis and periodontitis can impact overall health, but periodontitis poses a greater risk due to its association with systemic conditions. Chronic inflammation from advanced gum disease has been linked to heart disease, diabetes, and complications during pregnancy, making timely intervention critical.
Prevention and Best Practices
Oral Hygiene Routine
The foundation of gum disease prevention lies in maintaining a consistent oral hygiene routine. Brush your teeth for at least two minutes twice daily using fluoride toothpaste. Floss daily to remove debris and plaque from between teeth, and consider using an antimicrobial mouthwash to kill bacteria.
Regular Dental Visits
Professional cleanings and check-ups are essential for early detection and treatment of gum disease. Dentists can remove tartar that cannot be eliminated through brushing and identify early signs of gingivitis before it progresses.
Lifestyle Adjustments
Healthy lifestyle choices, such as quitting smoking, reducing sugar intake, and consuming a balanced diet rich in vitamins and minerals, can significantly lower the risk of gum disease. Stress management also plays a role, as stress can weaken the immune system and exacerbate oral health issues.
Monitoring and Maintenance
Pay attention to your gums—look for redness, swelling, or bleeding signs. Regularly replace your toothbrush and ensure it has soft bristles to avoid damaging your gums. Promptly address any concerns with a dental professional to maintain long-term oral health.
Conclusion
Understanding the differences between gingivitis and periodontitis is essential for optimal oral health. While mild and reversible, gingivitis can progress to periodontitis if neglected, causing irreversible damage to the gums and teeth. Prevention through good oral hygiene, regular dental visits, and a healthy lifestyle is key to avoiding these conditions. By staying informed and proactive, you can protect your gums and enjoy a lifetime of healthy smiles.
FAQs
- What are the first signs of gingivitis?
- Red, swollen gums that bleed easily during brushing or flossing are early signs of gingivitis.
- Can gingivitis be reversed?
- With proper oral hygiene and professional cleaning, gingivitis can be reversed.
- How can I tell if I have periodontitis?
- Symptoms of periodontitis include gum recession, loose teeth, persistent bad breath, and gum abscesses.
- Is periodontitis curable?
- While it cannot be fully cured, periodontitis can be effectively managed with treatment and maintenance.
- How often should I visit the dentist to prevent gum disease?
- Visiting the dentist at least twice a year or more frequently is recommended if you are at higher risk.
You May Also Read: https://timebusinesswork.com/elizabeth-finfrock/

Leave a Reply